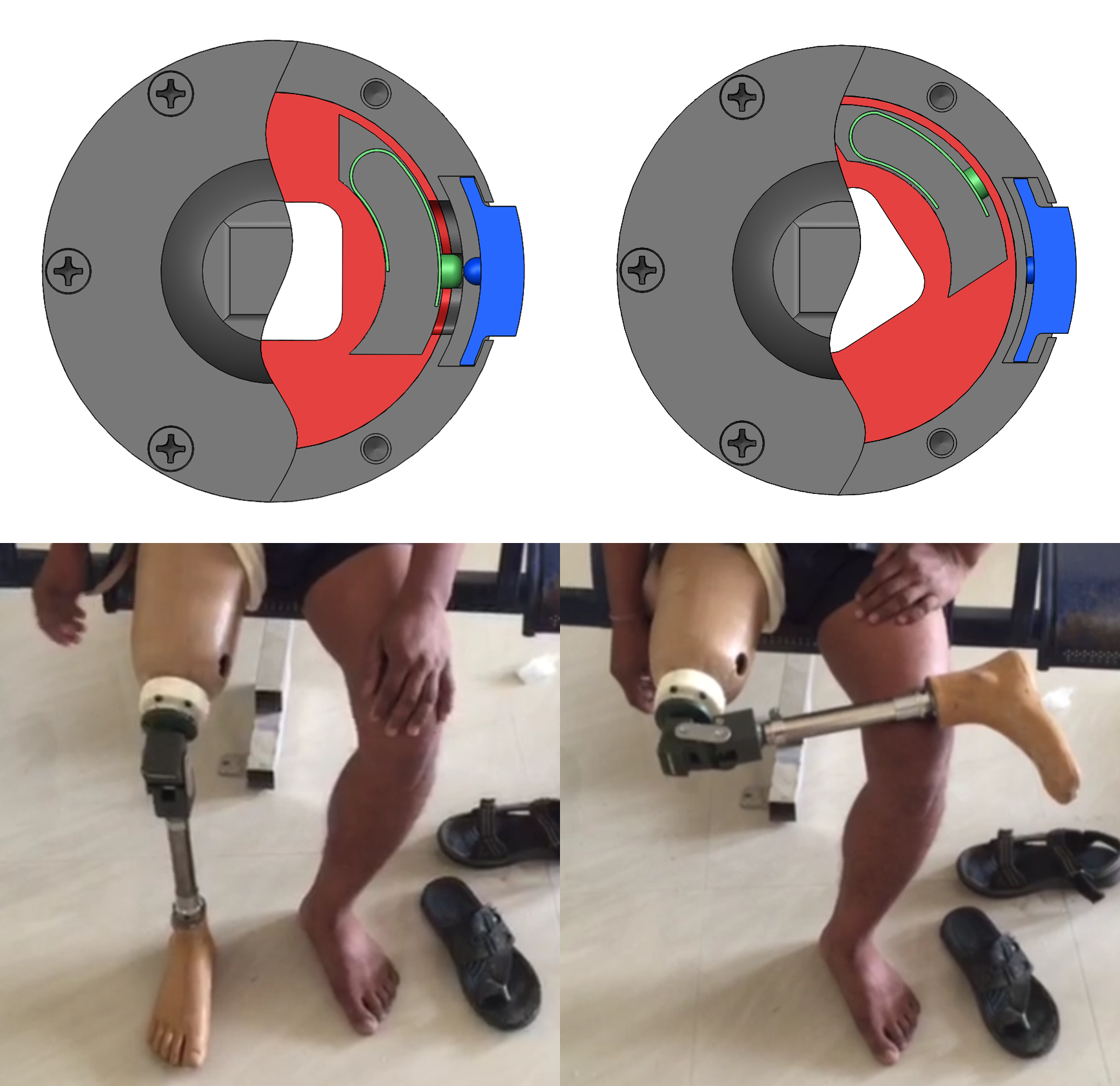
Fig. 1
Transfemoral amputees (those with above knee amputations) have particular difficulty crossing their legs. This is in part due to restriction of movement from the large socket and sometimes also in part a result of muscle loss through the amputation. While on the surface this may seem like a minor inconvenience, being able to cross one's legs can be advantageous. For example, it can aid in tying ones shoes, ingress and egress from vehicles, cross legged sitting on the ground, and perhaps most importantly in some parts of the world, the ability to blend in and hide the fact that they are an amputee.
Fig. 2
All this can be accomplished through the use of a transfemoral rotator, which sits above the prosthetic knee. Typically unlocked with a button, they then allow the lower part of the prosthesis to rotate into the desired position. While a few rotators already exist in the developed world, they are very complicated and can cost thousands of dollars. Thus, they have never made it to being introduced in the developing world. Therefore, the goal of this project was to design a low cost (sub $10) and robust rotator to be used in India with the current Standford-Jaipur knee in figure 2. Why India and why the Standford-Jaipur Knee? India was chosen due to the many cultural customs of sitting cross-legged and the social stigma surrounding amputees. Thus anything, allowing amputees in India to better blend in and participate in cultural practices, is likely to be adopted. This particular knee was chosen due to its unprecedented low cost (~$20) and durability.
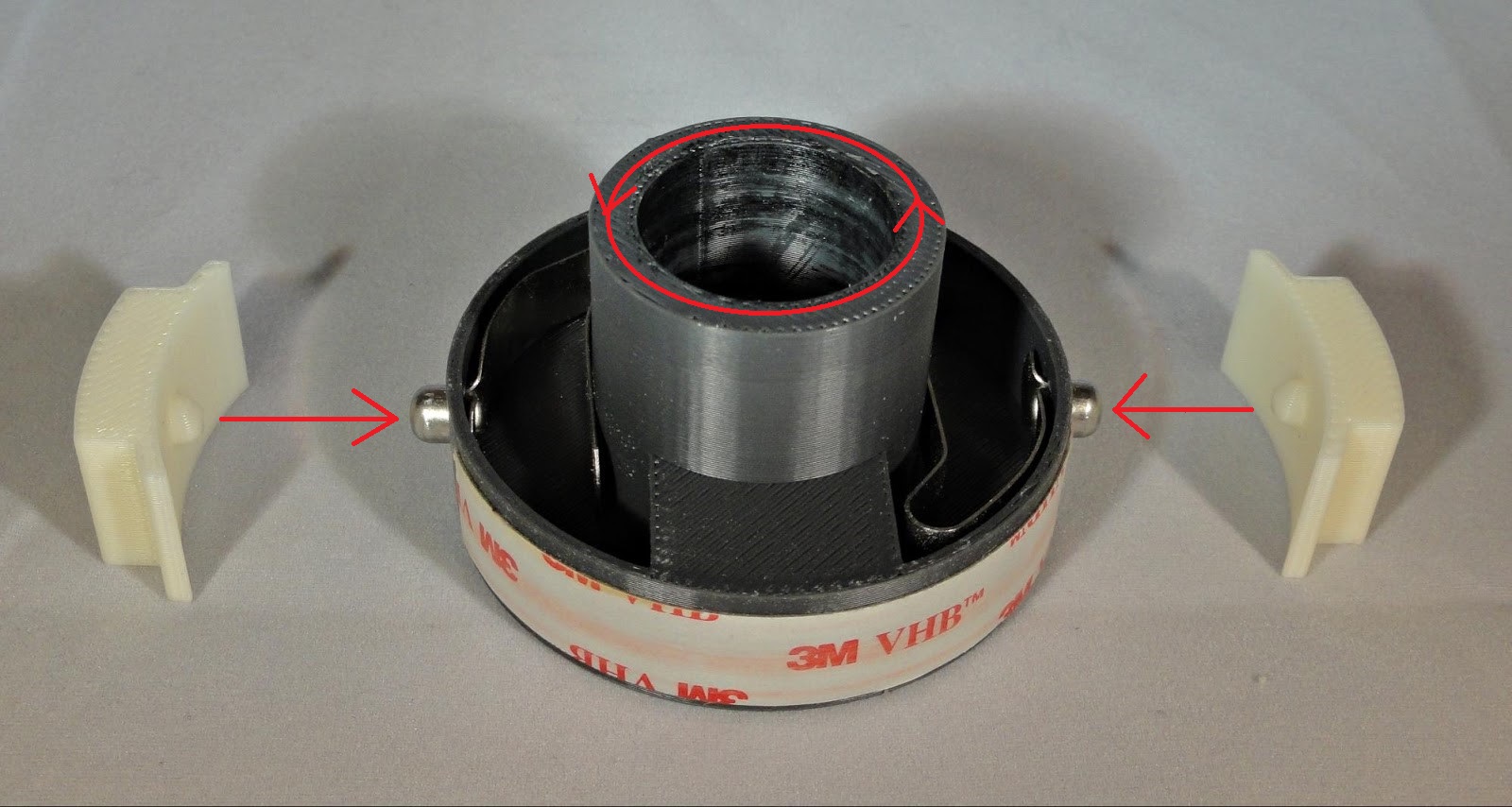
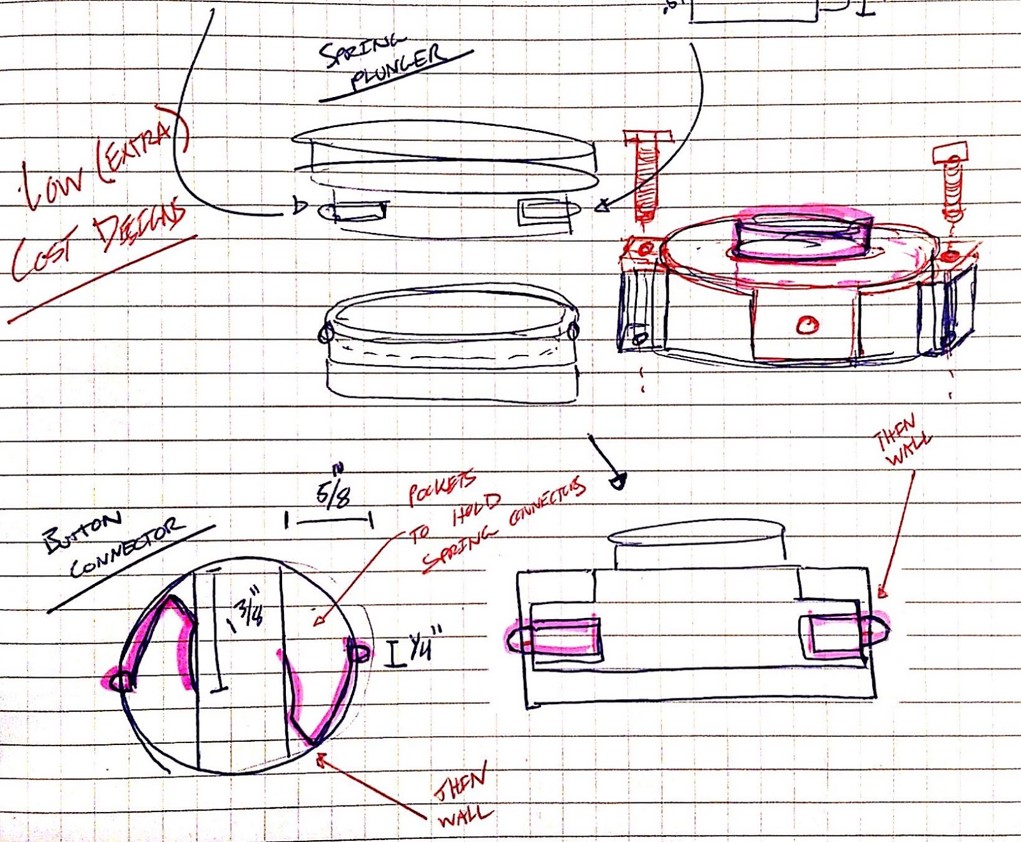
Fig. 3
The initial concept for my solution came from tube connector mechanisms as shown in figure 3. Using these cheap and readily available tube connectors (or push button spring clips) helped to simplify and lower the cost of the device. Essentially, the tube connectors would lock together an inner cylinder (attached to the lower prosthesis and top of knee joint) and a concentric outer cylinder (attached to the upper prosthesis and socket). Through 3D printed iterations, large buttons were added to make depressing the tube connectors (and subsequently disengaging the lock) much easier, especially through pants. Furthermore, interfacing with the knee and socket was accomplished consistently with the current Stanford-Jaipur Knee through large screws.
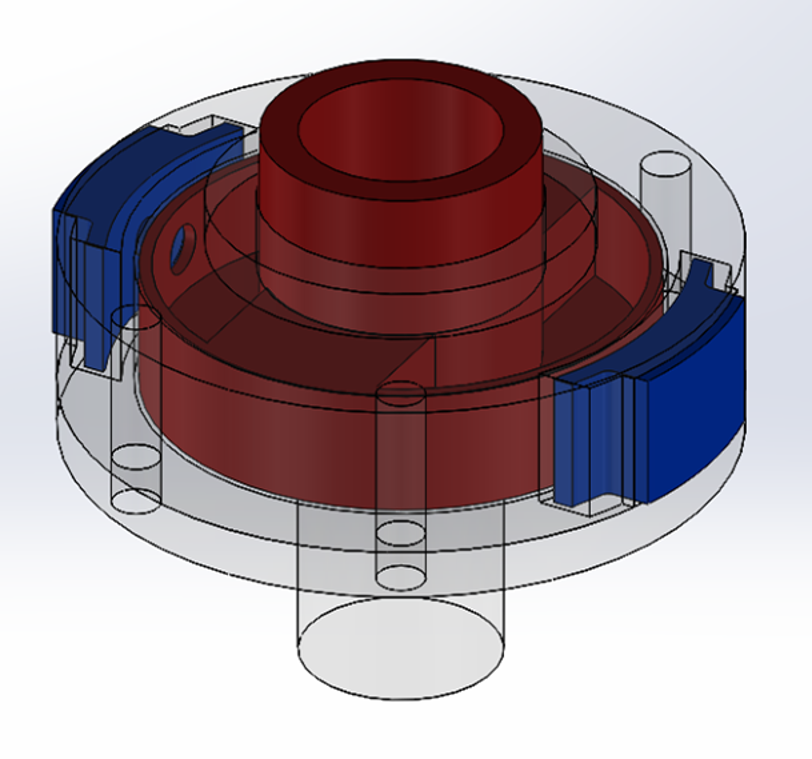
A more in depth look at the design (Fig. 5 and 6) shows that the rotator is composed of an inner cylinder (red), a split outer casing (dark gray and transparent), two buttons (blue), and two push button spring clips (green). When the buttons are depressed, the push button spring clips are forced through the holes in the casing wall, allowing the inner cylinder to rotate freely. So long as the two buttons remain depressed, the inner cylinder, which is attached to the distal prosthetic leg assembly, is allowed to rotate 360degrees. If the buttons are released after the initial unlocking, the inner cylinder will lock in place after 180 degrees of rotation as the push button spring clips reengage the holes in the casing wall.
Fig. 4
As for the manufacturing process, all parts are either cheaply machined or purchased for a total cost of under $10. Furthermore, all parts can be easily integrated into Jaipur Foot's current manufacturing process. The only functional requirement that was not met was the ideal height of less than 1.25 inches (height of current rotators). Fortunately, however, Jaipur Foot put concerns over the height to rest, citing the fact that the length of residual limbs varies so much that the actual height of the rotator is not nearly as important as its stability and longevity.
Update: I am traveling in January 2016 to Bangalaru and Jaipur, India, to test the rotator with Mobility India and Jaipur Foot respectively -- two companies based in India that focus their efforts on developing and delivering low cost prostheses to impoverished amputees. This trip will hopefully identify ways to improve the rotator and set in motion the process towards production of this device. I also hope to learn more about prostheses in the developing world and get a better idea for patient need and how it differs from previous work I've done in the developed world.
Fig. 5
Fig. 6